How Clomiphene and Letrozole Work Differently
Clomiphene often behaves like a loud coach shouting at the brain: it binds estrogen receptors in the hypothalamus so the body senses low estrogen, boosting GnRH pulses and FSH release to coax follicles awake. Letrozole feels more like turning down estrogen production itself by blocking aromatase, lowering circulating estrogen and indirectly lifting FSH without the receptor blockade; this leads to subtler endocrine shifts and different uterine responses and ovarian dynamics.
Clinically these mechanisms mean differing side effects and monitoring needs: clomiphene’s receptor antagonism can thin the endometrium, cause visual disturbances or mood swings, and may rarely lead to multiple gestations. Letrozole’s estrogen suppression tends to preserve the lining and usually produces fewer hot flashes, though lipid changes and bone density effects deserve attention with prolonged use. Teh choice depends on prior response, age and patient preference after clinician discussion carefully.
| Agent | Primary Action |
|---|---|
| Clomiphene | Estrogen receptor modulation (hypothalamic blockade) |
| Letrozole | Aromatase inhibition (reduces estrogen synthesis) |
Comparing Ovulation Induction Success Rates in Patients

She watched two months pass and learned to time hopes with tests; each pill felt like a small wager. Clinicians often start with clomiphene because it's familiar, low-cost and well-studied, but newer aromatase inhibitors introduced a shift in expectations for ovulation and pregnancy outcomes.
Randomized trials and meta-analyses show that letrozole often produces higher ovulation and live-birth rates in certain groups, notably women with polycystic ovary syndrome. Success is influenced by age, BMI and prior response; responders to clomiphene may still do well, but nonresponders are definately more likely to benefit from switching.
Clinicians weigh cumulative conception rates across cycles, side-effect profiles and patient preference when choosing therapy. For many, a trial of oral agents with ultrasound monitoring is a logical first step; timely switch to alternative agents or assisted techniques raises overall chances, creating a tailored journey toward pregnancy.
Side Effects Profile Short Term Versus Long Term
Short-term side effects often feel familiar: hot flashes, mood swings, and breast tenderness. Patients taking clomiphene also report visual disturbances or bloating, usually resolving after a few cycles.
Letrozole’s short-term profile leans to fatigue and joint pain, but tends to be milder and briefer for many. Monitoring and dose adjustments reduce bother and improve tolerability.
Long-term concerns are subtler: repeated clomiphene cycles may thin uterine lining or affect cervical mucus, potentially impacting implantation. Evidence on teratogenic risk is reassuring but not exhaustive.
Letrozole’s longer-term effects are less defined; studies suggest similar live-birth rates and no clear increase in birth defects. Discussing goals and history with your clinician helps acomplish safer choices for individualized patient treatment.
Safety Considerations for Specific Patient Populations

Patients with differing health backgrounds respond differently to ovulation agents. Women with liver disease, uncontrolled thyroid dysfunction or thromboembolic disorders require alternate strategies and evaluation before treatment. For those with estrogen-sensitive cancers, clomiphene may be avoided and oncology input sought.
Cardiovascular disease, clotting diatheses and severe obesity raise safety concerns; clomiphene's estrogenic modulation can be particularly problematic. Specialists monitor for ovarian hyperstimulation and multiple gestation; Occassionally ultrasound and hormone checks are neccessary to adjust dosing.
Older patients and those with prior pelvic surgery or endometriosis need tailored protocols, informed consent about off-target effects, and prompt reporting of visual symptoms or pelvic pain. Shared decision-making, access to emergency care, and a clear follow-up plan minimize risk.
Practical Treatment Protocols: Dosing, Timing, Monitoring
A hopeful patient begins with a clear, individualised plan: clomiphene often starts on cycle days 3–7. Teh clinician sets dose, tracks follicles and adjusts based on response.
Timing focuses on ovulation prediction via serial ultrasounds and luteinizing hormone tests; insemination or timed intercourse is scheduled accordingly. Blood work checks estradiol and progesterone to ensure safety.
Monitoring continues for side effects and multi-follicular development; dosage may be increased in subsequent cycles or switched if response is inadequate. Clear communication, consent and follow-up make protocols effective.
| Dose | Timing |
|---|---|
| 50 mg | Day 3 |
Choosing between Drugs Cost Accessibility Patient Preference
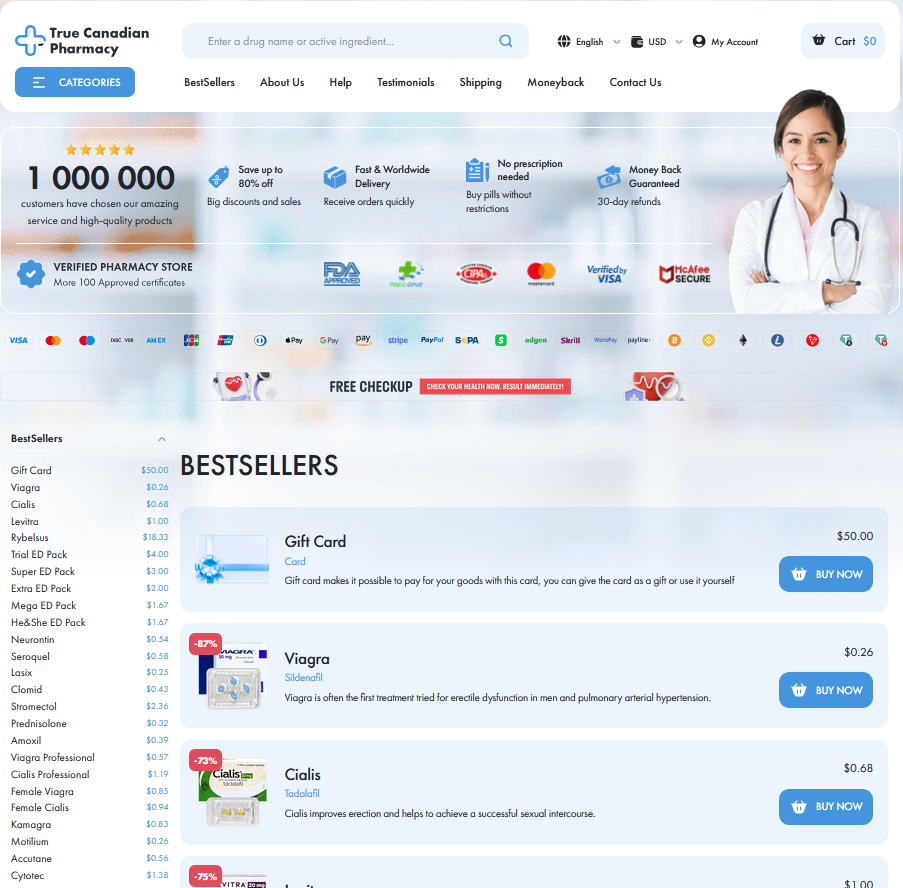
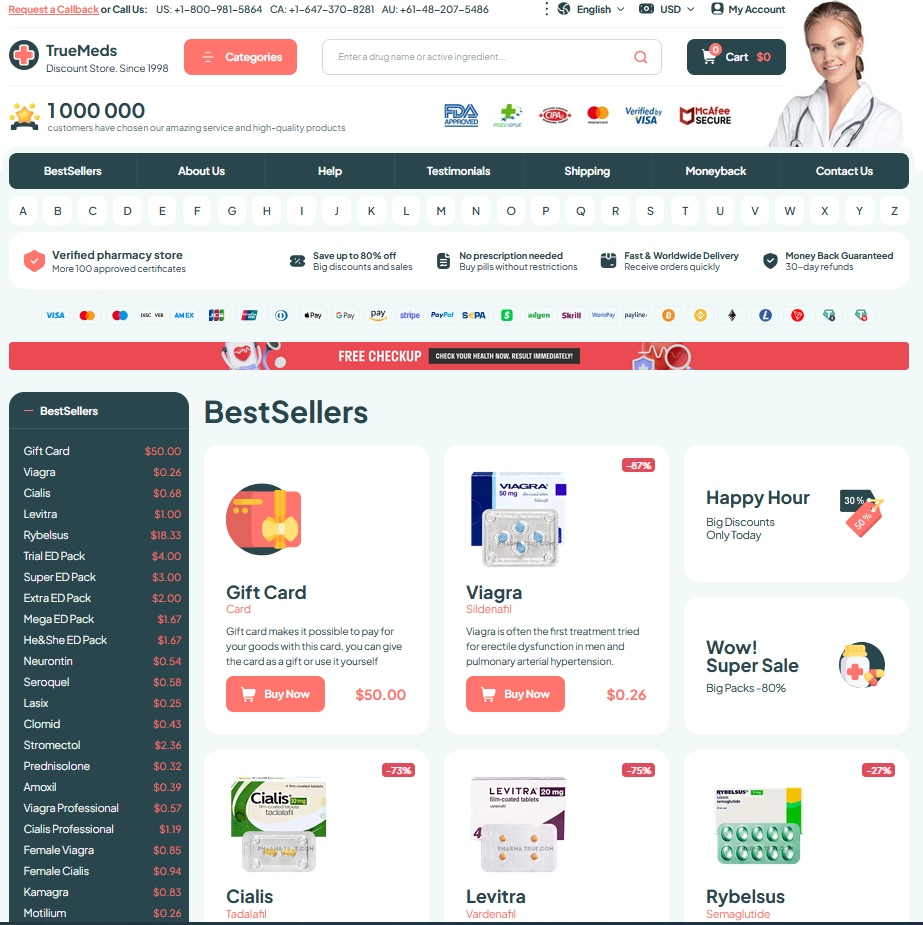
Clinic conversations often turn to price and convenience. Insurance coverage, copays and local pharmacy stock can nudge decisions. A pragmatic approach also weighs immediate cost against expected success and follow-up needs.
Access varies: clomiphene is widely available as an inexpensive generic, while letrozole may need specialty pharmacies or prior authorization. Travel, lab monitoring and clinic visits add hidden costs to discuss with your provider.
Patient preference matters: tolerance of side effects, desire for fewer clinic visits, or concerns about long term risks influence choices. Shared decision making lets couples weigh personal values, success probabilities and quality of life tradeoffs.
Clinicians can often recomend a cost-effective pathway: start with an affordable, monitored trial, reassess after a few cycles and move to alternative agents if needed. Factor in fertility goals, time horizon and insurance coverage. PubMed: clomiphene Cochrane Library: clomiphene